When you think of “Mind-Body Medicine”, what do you think of?
Most people who aren’t in the healthcare profession usually have no clue what that means, let alone how it would benefit them and their loved ones. The question is usually followed with a blank stare and a slow nod of the head.
So, I thought it would be helpful to give you a solid foundation regarding the key aspects behind mind-body health and healing. In doing so, I’ve created a 5-Part Mind-Body blog series to introduce you to this emerging field. For part 1 of the series, I will be addressing the importance of the limbic brain and the HPA-axis in mental and physical health. Warning – This can get a bit dense in scientific terms. So, sit back, relax, and allow me to break it down for you as simply as possible…
“Mind-body medicine” is a field that explores how one’s thoughts, emotions, spiritual experiences, and dreamtime experiences can stimulate a physiological response within the body.
How does obsessive fear-based thinking affect one’s physical health? How does mania and psychosis affect one’s physical health? How does disordered thinking about food, sex, finances, relationships, etc. affect physical health? How do traumatic events and memories affect physical health? How does insomnia affect physical health? Well – in any case, all dysfunctional emotional or thought processes are interpreted as stress by the body. No matter if you’re experiencing grief, anger, fear, lack of sleep, spiritual disconnection, or unhealthy relationships – it’s all interpreted as stress.
Now, let’s be real. Experiencing stress is a normal part of life. Every person will experience moments in his/her/their life that are stressful. Some people are able to bounce back quicker and more gracefully than others. Others may need more time and support. Ultimately, every human being has the ability to heal and move through these experiences. Stress, however, becomes maladaptive when we stay stuck in a certain way of thinking or feeling. An even greater signal that stress has become maladaptive is when it begins to manifest as an illness – whether it be mental or physical.
So, where does this maladaptive process begin? Well, modern research in neuroscience and neuropsychiatry has shown that one aspect of this maladaptive process begins in a structure within the brain known as the limbic system that signals a hormonal pathway, known as the HPA-Axis.
What exactly is the limbic system?
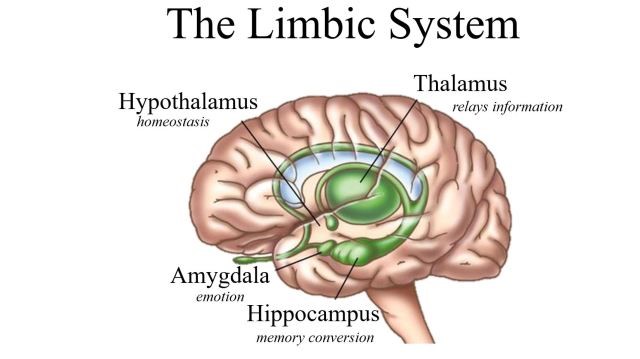
It is the part of the brain associated with behavioral and emotional responses, especially responses necessary for survival: feeding, reproduction, child rearing, and the fight or flight response. It contains the thalamus, the hypothalamus, the basal ganglia, the hippocampus, and the amygdala.
The thalamus is the relay center of the brain. It is important for organizing signals and sending them to their respective parts of the brain.
The hypothalamus is important for hormone production and the regulation of thirst, hunger, mood, blood pressure, and more. I’ll go into more depth about this particular structure in just a moment.
The basal ganglia is responsible for reward processing, habit formation, movement, and learning.
The hippocampus is essentially the memory center of the brain. Here is where memories are formed and stored, both conscious and unconscious. It contains neurons that extend into the cerebral cortex to help us associate certain memories with our physical senses (i.e. being reminded of loved ones upon hearing certain songs). Along with memory formation, the hippocampus is one area within the brain where new neurons are created, providing us the ability to learn new things (such as, new ways of perceiving the past, or new behaviors). This ability to generate new neurons is known as “neurogenesis”, while the phenomenon of creating new neurons as a result of learning new things is known as “brain plasticity”. We will dive into these two topics in a later blog post.
The amygdala plays a central role in our emotional responses including pleasure, fear, and anger. It also attaches emotional content to our memories and therefore plays a crucial role in discerning how robustly those memories are stored. In other words, memories that have a strong emotional meaning tend to stick more. So, if we hear a song that reminds us of someone we love, we may begin to feel joy, sadness, or gratitude – depending on the nature of the relationship. Memories that are especially traumatic can be so incredibly emotional, that they are filed away deep within our subconscious – to be consciously forgotten, until a triggering event brings that memory back to one’s conscious awareness. Often times, the triggering memory can cause an immediate “fight or flight” response.
What exactly is the “fight or flight” response?
The fight or flight response, or the acute stress response, is a physiological reaction in response to a perceived harmful event or threat to survival. It prepares our bodies to either stay and fight, or to run away. It is normal for all living things, including plants and insects, to experience short-term stress, and eventually let it go. However, as humans, our bodies also overreact to non-life-threatening situations, such as, school and work pressure, traffic jams, family disputes, and more. Repeated activation of this stress response can have ill effects on the body.
So, how is all of this connected?
Chronic, emotional stress leads to repeated activation of the “fight or flight” response in the hypothalamus. It triggers persistent production of CRH (corticotropic-releasing hormone) in the hypothalamus and glucocorticoid receptors at sites all over the body.
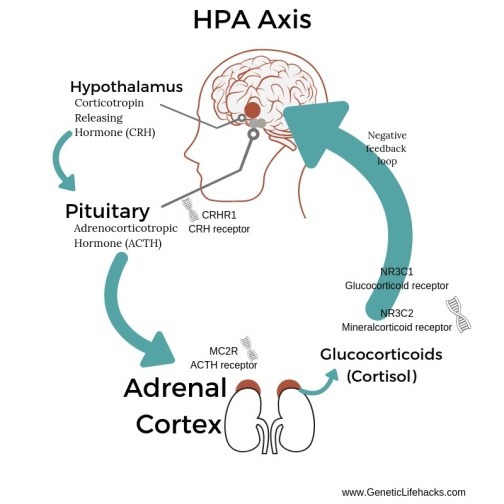
One important pathway is the HPA-axis (called the hypothalamic-pituitary-adrenal axis). It is what connects the central nervous system to the endocrine and immune systems. The stress response initiates the release of CRH from the hypothalamus into the anterior pituitary gland, which then releases ACTH (adrenocorticotropic hormone) to the adrenal glands for the production and release of cortisol.
The released cortisol travels throughout the bloodstream and binds to glucocorticoid receptors on cells all throughout the body, resulting in the following:
- reduced insulin production and release
- elevated blood glucose
- elevated blood pressure
- an increased risk of ulcers and infections within the digestive tract
- increased bone mineral loss
- a suppressed immune system (which disables your ability to combat and remove infections and toxins)
- unwanted weight gain
- and more
So, with all of that said – it’s no coincidence how a dysfunctional HPA-axis can directly cause, or at least be associated with, many cases of adrenal insufficiency (commonly known as “adrenal fatigue”), metabolic syndrome, diabetes, cardiovascular disease, digestive concerns, such as, peptic ulcers and dysbiosis, chronic infections, osteopenia/osteoporosis, an inability to lose weight, and more.
So, let’s now shift to common mental illnesses: behavioral disorders, eating disorders, depression, anxiety, bipolar disorder, trauma, addiction, and even personality disorders. Given the connection between the limbic system and the HPA axis, we can see how the mind’s ability to create and store negative memories, as well as, dysfunctional behavioral patterns and emotional responses can impact our physical health.
This is why when treating patients with mental illness, or even patients who simply report an inability to work through difficult emotions, experiences, and patterns, it is important to treat ALL aspects of the individual.
My approach to holistic healing integrates both naturopathic and traditional Afro-diasporic perspectives:
- providing referrals for in-depth counseling and psychotherapy
- encouraging healthy social relationships (including a healthy relationship with yourself)
- encouraging some type of spiritual or moral support (i.e. support groups, spiritual organizations, ritual, church service, etc.)
- establishing proper sleep hygiene (including the integration of dreamwork)
- encouraging a daily meditative practice to reduce stress and ground yourself
- promoting adequate physical activity (whatever that may look like for you)
- enhancing your body’s own inherent vital force using nutrition, homeopathy, hydrotherapy, herbs, and craniosacral therapy
- supporting weakened organs and/or systems as a result of a dysfunctional HPA axis using nutrition, hydrotherapy, and herbs
My services will be available beginning this October at The Center: A Place of Hope in Washington, which is an in-patient treatment facility for various mental illnesses, eating disorders, and addictions. For more information about the services I will be offering, or how to arrange accommodations at The Center, you may contact me through my website’s Contact Page (click here).
Be sure to like and follow my facebook page and/or my instagram page to stay updated for next week’s Part 2 of the Mind-Body Series, “The Vagus Nerve and the Social Nervous System”, where I will be discussing the role of the vagus nerve in the development and expression of empathy, and the “fight or flight” response.
Until next time,
Dr. Richmond
Remaining Posts of Mind-Body Series:
- The Vagus Nerve and the Social Nervous System (Next Week)
- The Gut-Brain Connection
- The Green Mind Theory
- The Neurobiology of Spirituality
Picture References:
- http://www.pbs.org/wgbh/pages/frontline/shows/teenbrain/
- https://www.geneticlifehacks.com/hpa-axis-dysfunction-genes-and-environment/